In December 2019, Duke University performed the US’ first heart transplant from a donation after circulatory determination of death (DCD) case. Prior to this announcement, the preferred donor for hearts was a donor after neurologic determination of death (DND). There were concerns about the risk of warm ischemic damage to the cardiac tissue throughout the dying process and death and up to the time of heart recovery; and there was no way for physicians to assess the heart function prior to utilizing it for transplantation.
The creation of new perfusion machines, the use of which have been well established in kidneys, significantly increasing kidney usage for transplantation, were now emerging for the lungs, heart and most recently the liver. In other countries, these perfusion machines had already been utilized with promising results. The US’ approval of the use of these perfusion machines were the key to opening the door to pursuing DCD heart recovery.
Today, there are several perfusion options and more in development. The first heart perfusion machine, Organ Care System (OCS) Heart is “a portable, warm perfusion, and monitoring system designed to keep a donor heart at a human-like, metabolically active state”, according to Transmedics. By placing the DCD heart onto the OCS (ex situ, i.e. outside of the human body) the heart can be successfully resuscitated, preserved, assessed and possibly reconditioned prior to transplantation (Qin et al, 2022).
Normothermic Regional Perfusion (NRP)
Another approach to facilitate improved organ function post cessation of circulation in a DCD case, is the use of Normothermic Regional Perfusion. Some have described the use of NRP as an innovation facilitating the stewardship of the gift of the donor.
Normothermic regional perfusion (NRP) is an in situ perfusion of a portion of the donor’s body with the help of extracorporeal organ support (ECOS).
In live patient care (non-donation situations), ECOS artificially supports lung and or heart function by using a machine that oxygenates a patient’s blood outside of the body and returns it to the patient through the use of a pump. Utilizing this machine allows the heart and lungs to rest and therefore can promote healing of organs (UCSF Fresno). ECOS is regularly utilized in cardiothoracic care of critical patients. (In live patient care, it may be called extracorporeal life support ‘ECLS’.)
The use of ECOS in DCD allows for circulation to be re-established after cardiac cessation has occurred and a certain “hands-off” period (typically 5 mins) was observed prior the first incision being made. The re-established circulation will be limited to a specific area of the body, either isolated to the abdominal area (A-NRP) or both in the abdominal and thoracic area (TA-NRP). Hence the term “regional perfusion”, indicating the perfusion is facilitated with the help of the ECOS in a specific region of the body, excluding the brain or brain stem. 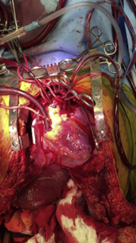
To keep the perfusion ‘regional’, after the sternotomy and a pericardiotomy has been performed, the arch vessels (including the cerebral arteries) are clamped and vented to prevent brain perfusion, and the aorta and right atrium are cannulated to allow for initiation of the circulatory support. (For a more detailed description read Shah’s article 2022.)
The recipients and donor families are respectively informed of the use of the new technique and details of the procedure are shared if they wish for more specific information.
Early results of this new technique are mirroring the findings of other countries, such as UK, France, Italy, and Spain, who have a few more years of experience in performing this procedure. The hearts are being transplanted with positive results, adding a significant amount of hearts being available for those who are in desperate need of transplant. An additional early positive finding, such as described by Sellers et al. (2022), is the improved liver function of the donated liver following the use of NRP, which may also increase the number of livers available for transplant.
Ultimately, the use of NRP and perfusion devices can facilitate better outcomes and improvement in the stewardship of the gift that the donor and their family have made.