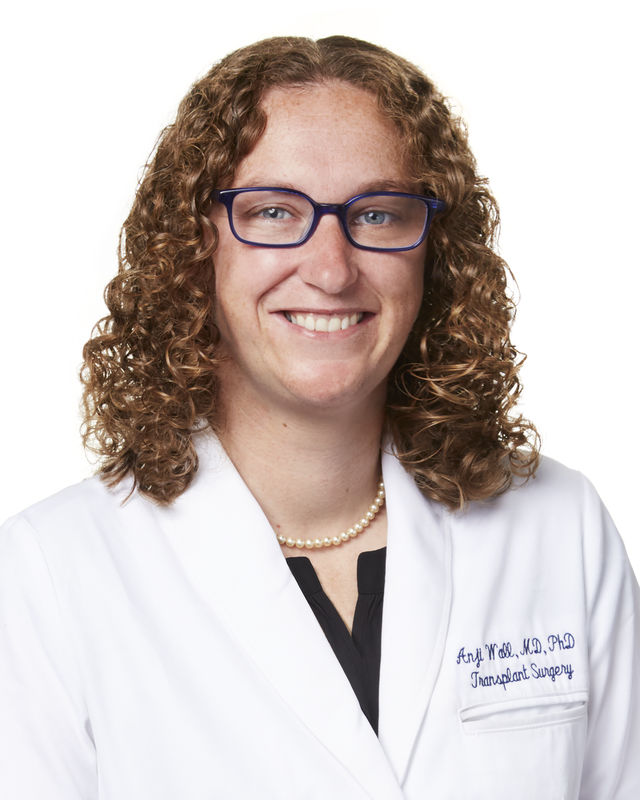
Anji Wall is an abdominal transplant surgeon and bioethicist at Baylor University Medical Center in Dallas, TX. She is the vice chair of research at the Baylor Simmons Transplant Institute. Her research interests include transplant policy ethics, ethical and clinical questions in uterus transplantation, and perceptions of waitlisted patients regarding different types of donors. Her clinical practice focuses on deceased and living donor liver, kidney and uterus transplantation.
Normothermic regional perfusion (NRP) is an innovative approach to maintaining organ viability following the determination of circulatory death (DCD). The comprehensive and collaborative approach required to facilitate an NRP recovery has increased organ utilization while reducing waitlist deaths. In this session, we will be joined by leaders in the community who will share their respective journeys to NRP implementation in partnership with their local OPO or receiving Transplant Center(s). Methods on how to engage key stakeholders will be shared along with examples of how to overcome potential barriers, resulting in more lives saved through this increasingly prevalent method of procurement.