Community Hospital
Resource Guide
A vital guide for hospital senior leaders to develop impactful organ, eye and tissue donation practices
Table of Contents
A Community Hospital Resource Guide
For linking to the Community Resource Toolbox, the Community Hospital Resource Guide and Transplant Quality Resources Guide and Tools, please use the following disclaimers:
Community Resource Toolbox Disclaimer:
The Community Resource Toolbox includes a variety of resources created, collected, and/or compiled by the Organ Donation and Transplantation Alliance. (Insert name of your organization) is neither affiliated with nor endorsed by the Alliance and claims no ownership in any of the Community Resource Toolbox materials. By clicking this link, you will be directed to the Alliance’s website located at https://www.organdonationalliance.org//resources/toolbox/.
Please use the Alliance logo on your website. Link here to locate and download a version of the logo that best suits your site:
Transplant Resource Guide (TRG) Disclaimer:
The Transplant Resource Guide (TRG) includes a variety of resources created, collected, and/or compiled by the Organ Donation and Transplantation Alliance. (Insert name of your organization) is neither affiliated with nor endorsed by the Alliance and claims no ownership in any of the Transplant Resource Guide (TRG) materials. By clicking this link, you will be directed to the Alliance’s website located at https://www.organdonationalliance.org/resources/transplant-resource-guide/.
Please use the Alliance logo on your website. Link here to locate and download a version of the logo that best suits your site:
Community Hospital Resource Guide Disclaimer:
The Community Hospital Resource Guide includes a variety of resources created, collected, and/or compiled by the Organ Donation and Transplantation Alliance. (Insert name of your organization) is neither affiliated with nor endorsed by the Alliance and claims no ownership in any of the Community Hospital Resource Guide materials. By clicking this link, you will be directed to the Alliance’s website located at https://www.organdonationalliance.org/resources/community-hospital-resource-guide/.
Please use the Alliance logo on your website. Link here to locate and download a version of the logo that best suits your site:
The Alliance Resource Section
ESSENTIAL 4
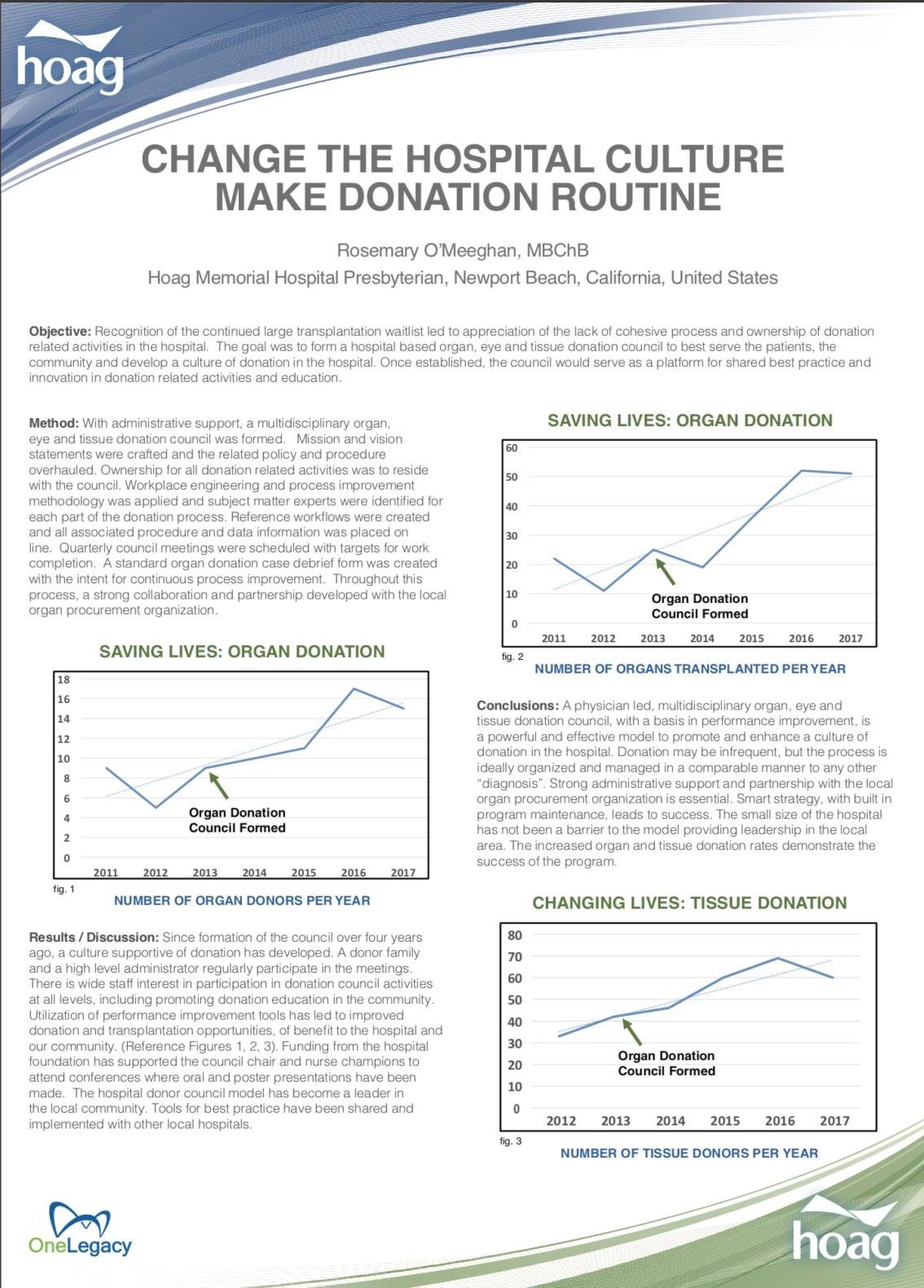
Creating a Culture of Collaboration
This essential demonstrates the power of collaboration between the hospital and the OPO. By engaging key stakeholders from the hospital and identifying donation champions to communicate and strategize with the OPO, there is potential to reach incredible efficacy toward donation education, recognition of clinical triggers, patient referral and donor outcomes. A donation council or other hospital meetings may serve as an excellent collaborative forum to enhance communication among hospital teams and the local OPO.
Fact Finding Questions CEOs May Ask of Their Senior Leadership:
- What are our institutional clinical triggers for referring a patient with a catastrophic brain injury or non-survivable illness/injury to the OPO, and/or when families are considering withdrawal of life-sustaining treatments?
- What are we doing to follow the effective request process?
- Who are our donation champions? Are various disciplines represented?
- Do we have regular meetings and reviews with the OPO? Do we have a donation council?
- What are we doing to ensure the OPO has access to our EMR system?
Model Elements for Creating a Culture of Collaboration
Detailed Components for Creating Culture of Collaboration
- Local Donation Service Area (DSA) annual small hospital senior leadership meeting (hold an honest discussion with OPO leadership on frequently encountered issues, areas of opportunity and successful practices).
-
- Premature assumptions of outcomes by clinicians (i.e., assumptions that patient isn’t going to survive; OPO would not be interested; family will interfere).
- Personal bias/assumptions on what the patient would want.
- CEO to ask their team if they do this:
- How often do you withdraw care in the ED?
- How often do you pronounce death in the ED?
- What is your referral practice?
- Identify donation champions.
- Model elements for construction of donation councils- and how they relate to and integrate with other existing hospital committees/groups.
- Integration of QI representatives and resources to the collaborative meetings, e.g. donation council, to aid data review, provoke reflection, and help define change goals .
- Define expectations of activity of the donation council (e.g.-Donate Life Month Activities).
- Employ model communication practices.
- Set goals related to collaboration and evaluate performance.
-
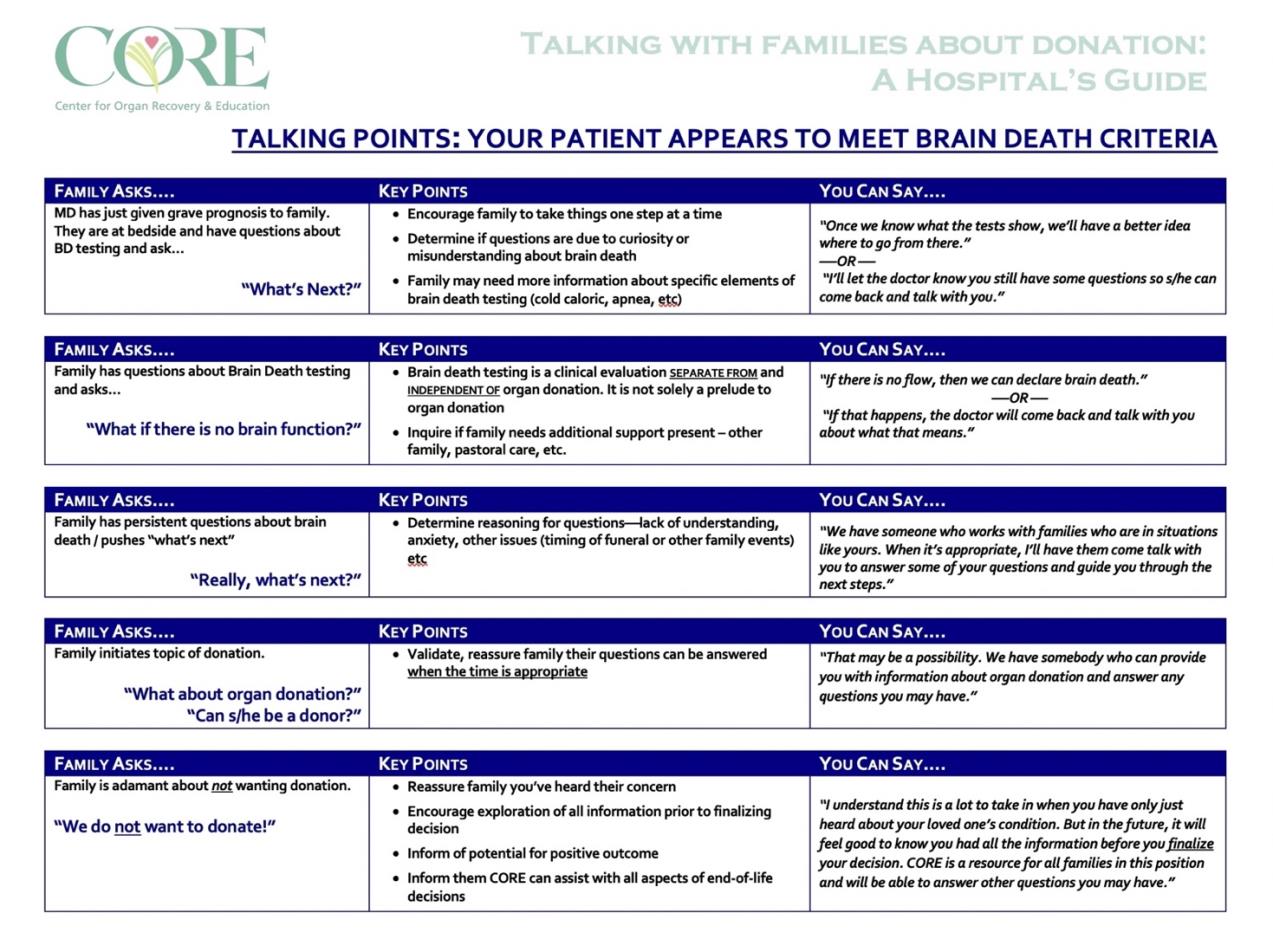
- Formatted Communication Examples (Scripting for Families) [Appendix 21]
- Changing Hospital Culture and Making Donation Routine [Appendix 24]
- Model Elements of a Donation Council [Appendix 19]
- Example Organ, Eye, and Tissue Donation Committee Policy Statement [Appendix 20]
- Fast Facts and Plain Language Planner
Optimal donation process should be documented in an Affiliation Agreement or Memorandum of Agreement (MOA) between the hospital and OPO. CMS §482.45 Condition of Participation: Organ, Tissue and Eye Procurement
Hospitals must have and implement written protocols that addresses its regulatory and accreditation standards, organ donation responsibilities.
Affiliation Agreement and written protocols must include:
- Hospitals must notify the OPO of every death or imminent death in the hospital. When death is imminent, the hospital must notify the OPO both before a potential donor is removed from a ventilator and while the potential donor’s organs are still viable. The hospital should have a written policy, developed in coordination with the OPO and approved by the hospital’s medical staff and governing body, to define “imminent death.”
- Hospitals and their OPO should develop a definition of “imminent death” that includes specific triggers for notifying the OPO about an imminent death
- “Timely notification” is defined in the MOA or Affiliation Agreement
- It is the responsibility of the OPO to screen for medical suitability of potential donors. Once the OPO has identified a potential donor, that person’s family must be informed of the family’s donation options.
- The OPO and the hospital will decide together how and by whom the family will be approached.
- Hospital ensures that the family of each potential donor is informed of its options to donate organs, tissues, or eyes, including the option to decline to donate.
- The individual appointed by the hospital to initiate the request to a family must be an organ procurement representative, an organizational representative of a tissue or eye bank, or a designated requestor. Any individuals involved in a request for organ, tissue, and eye donation must be formally trained in the donation request process.
- Using discretion does not mean a judgment can be made by the hospital that certain families should not be approached about donation. Hospitals should maintain a belief that a donation is possible and should take steps to ensure the family is treated with respect and care. The hospital staff’s belief that a family’s grief, race, ethnicity, religion or socioeconomic background would prevent donation should never be used as a reason not to approach a family.
- All potential donor families must be approached and informed of their donation rights.
- Reviewing medical records to improve identification of potential donors. Hospitals must cooperate with the OPOs, tissue and eye banks to ensure access for regular or periodic review of death records and, therefore, must develop policies and procedures which permit access that allow the OPO to assess the hospital’s donor potential, assure that all deaths or imminent deaths are being referred in a timely manner, and identify areas where the hospital sue and eye bank may improve donation performance measures.
- Maintaining potential donors while necessary testing and placement of potential organ, eye and tissues take place.
Details on a Donation Champion
A donation champion is defined as a person who takes extraordinary interest in the adoption, implementation and success of a cause, program or project. These individuals work to drive change despite internal resistance and will enthusiastically promote the program throughout the organization. As such they are a change agent and identifiable leader.
A champion for Organ, Eye and Tissue donation is well positioned in the role as chair of the multidisciplinary hospital Organ, Eye and Tissue donation council.
The champion and council should work to promote organization-wide awareness of and support for organ, eye, and tissue donation and to engage partners across departments. Multiple areas of the hospital can take part in the strategic planning and process improvement of the donation program. Education of council members allows them to become donation subject matter experts relative to their individual areas of practice in the organization.
Council activities led by the donation champion should focus on education and promotion of specific donation related activities in the hospital. For example, the senior hospital administrators may be provided with donation related data (e.g., imminent death referrals) and be educated to their role. This facilitates expansion of the program and assists with the development of a hospital culture of donation.
A close working relationship with the donation development coordinator from the local OPO is critical to the success of the program.
The donation champion may identify key stakeholders in multiple hospital areas such as:
- • Critical Care Units
- Operating Room
- Emergency Department
- Floor Manager, Supervisors
- Pharmacy
- Pastoral care & Social Workers
- Laboratory
- Nursing Education
- Respiratory Therapy
- QAPI
- Nursing Informatics
- Information Technology
- Public Relations / Marketing
- Medical Directors
- Nursing Directors
- Palliative Care
The donation champion can also liaise with and engage the hospital foundation, local civic administrators, donor family members and lead donor recognition events at the hospital. The donation champion can also partner with the local OPO to facilitate public education booths at local community events.
This outreach has the benefit of hospital wide participation – all are involved and have ownership. The culture of donation then extends to the communities that are served by the donation and transplantation process.
For hospital systems that have partner hospitals, there is the opportunity to collaborate on a regional basis with the goals to promote consistent organ, eye and tissue donation practices across the system. In this environment there can be sharing of best practice tools and processes, education about new donation practice (e.g. Hepatitis C and donation).
The donation champion is also well positioned to take part in and present at conferences and other donation related activities.
Qualities of a Champion
- Actively and enthusiastically promotes new change or innovation
- Is highly regarded in the organization
- Able to mobilize resources
- Able to navigate the socio-political environment within the hospital
- Skilled at building support for the change or innovation
- Ensures that change is implemented in face of organizational inertia or resistance
Model Elements for A Donation Council
Donation Council must include members of leadership that are impactful within the hospital system, preferably individuals that have a connection to and/or are passionate about donation and transplant.
Membership constituencies to include Critical Care, Palliative Care, Emergency Medicine, Neurosciences, Nursing, Hospital Senior Leadership/C-Suite:
- Attending MD (including Chief Resident and other trainees)
- Nursing, Nursing Educator
- Unit Clerk
- Palliative Care
- Pathology / Laboratory
- Admissions
- Security
- Public Relations / Marketing
- C-Suite (accountability, deviations to policy)
- Pastoral Care
- Respiratory Therapy
- Case Management / Social Work
- Pharmacy
- Ethics
- Medical Records
- Information Technology
- QAPI
- OPO Liaison
1. Content reviewed
- Referrals (timely and effective)
- Conversion
- Current donation promotion events
- Process breakdowns
- Deaths within an hour of WOLST
- Early WOLST
- Avoiding extubation prematurely (deeming “nonsurvivable” injuries vs. giving 72 hours)
- Criteria to go ahead with brain death declaration (drug metabolism vs. brain imaging)
- Pre-approach
- At a minimum, meetings should be held quarterly and potentially incorporated into other hospital/systemwide meetings
- Expectation is that council will take findings and disseminate information to their team
CMS GUIDELINES AND HOSPITAL COMPLIANCE
- Require that all potential donors must be offered the opportunity for donation. ALL families must have the opportunity to authorize or decline.
- Consider integrating QI reps and resources to aid data review, provoke reflection, and help define goals and OFIs/implementation.
- Often ask about donation activity.
- Organ Donation Legislation and Policy
DONATION COUNCIL ACTIVITY
- Can be quarterly and integrated into existing meetings in your institution or hospital system
- Quality End-of-Life Care/Legacy messaging and education
- Grand Rounds supported by donation council effort
- Post-donation debriefings for council
- Structured/consistent
- Timely
- Flexible (phone conference choice)
- Key individuals involved (direct care, supervisors, etc.)
- OPO communications for EVERY case that meets triggers in real time with entire council (e.g. SBAR-type status update), including administrators and key individuals
- Public Relations involvement to supply culturally sensitive promotion activities and determine how best to get information disseminated
- Opportunities for donation related events:
- February 14 is National Donor Day, April is Donate Life Month
- Examples of activities:
- Hospital Tabling Events (use volunteers to give information and obtain registration)
- Flag raisings ceremonies for patients who have donated organ, eyes, or tissue o Donor Memorial Wall events
EXAMPLE POLICY: ORGAN AND TISSUE DONATION COMMITTEE (DONATION COUNCIL)
Policy Statement
The Medical Staff of [INSERT HOSPITAL NAME] shall have a multidisciplinary standing committee responsible for directing and monitoring the Organ and Tissue Donation program across all [INSERT HOSPITAL NAME] hospitals and clinics. The name of this committee shall be the Organ and Tissue Donation Committee.
Scope
This policy applies to all members of the [INSERT HOSPITAL NAME] Medical staff, allied health professionals, residents, administration and employees, students, volunteers, and agency personnel who provide direct or indirect services to patients at [INSERT HOSPITAL NAME] hospitals and clinics.
Mission
- Treat any missed donor as an Event.
- Participate in increasing enrollment in the (OPO Name).
- Honor all first-person authorizations on deceased donors.
- Hold physicians accountable to complete brain death declaration regardless of family decisions about donation.
- Engage palliative care in family conversations about brain death.
- Collaborate with OPO to treat potential donors and prevent deceleration of care.
Purpose
- To develop, direct, and monitor the Organ and Tissue Donation program across all [INSERT HOSPITAL NAME] hospitals and clinics.
- To implement evidence-based Organ and Tissue Donation standards across all [INSERT HOSPITAL NAME] hospitals and clinics.
- To develop and make recommendations for approval of Organ and Tissue Donation policies and procedures across all [INSERT HOSPITAL NAME] hospitals and clinics.
- To promote improvement of quality indicators related to Organ and Tissue Donation practices across all [INSERT HOSPITAL NAME] hospitals and clinics.
Membership
- The physician Chair of the Organ and Tissue Donation Committee shall be appointed by the [INSERT HOSPITAL NAME] Chief of Staff.
- The Organ and Tissue Donation Committee shall include a physician representative from each Hospital campus involved in either Organ Donation by Brain Death Criteria or Donation after Circulatory Death. Members may also include other physicians including, but not limited to, hospitalists, intensivists, surgeons, anesthesiologists, and pulmonary specialists, appropriate OPO, Tissue Bank membership, Eye Bank membership, and other members as recommended jointly by the physician Chair and the [INSERT HOSPITAL NAME] Chief of Staff.
- Representatives from administration, nursing, and other proper clinical support areas shall serve as members. Non-physician representatives shall be appointed by the specific [INSERT HOSPITAL NAME] campus President or his/her designee, in collaboration with the [INSERT HOSPITAL NAME] Chief of Staff.
Expectations of Members
- To analyze and respond to data relevant to donation.
- To distribute donation data to all relevant individuals and departments.
- To take part in Organ and Tissue Donation Subcommittees and other project-related work.
- Mandatory attendance at all meetings or provision of proxy to attend in member’s stead.
Meetings
- The Organ and Tissue Donation Committee shall meet on a schedule determined in conjunction with the OPO based on donation potential and hospital needs.
- The Organ and Tissue Donation Committee shall prepare a record of attendance and keep minutes of its meetings, which record their actions and recommendations.
Reporting
The Organ and Tissue Donation Committee shall report pertinent findings to the [INSERT HOSPITAL NAME] Medical Staff Council.
Example 2: Reflective Listening and Open-Ended Questions
Reflective listening is an empathetic communication strategy that looks to genuinely understand the speaker’s concerns. People who receive reflective listening have reported more disclosure of feelings because they feel heard and accepted. Combined with open-ended questions, this type of strategy is beneficial when trying to engage a family in crisis and shock.
Reflective listening means rendering (transmitting) the speaker’s message using your own words and sentence structure. This shows the speaker that you have been listening to what they were saying. It creates trust and engagement between the speaker and listener.
Open-ended questions invite a family to elaborate, providing them with time and space to tell their story. They typically begin with “Why” and “How” or “Tell me about…” Oftentimes, open-ended questions are not asked as a question, but as a statement which implicitly asks for a response. Close-ended questions can be answered in only one word or a noticeably short phrase and have the potential to abruptly end the conversation.
Open ended questions are designed to:
- Encourage a full and meaningful answer using the family’s own knowledge and feelings
- Enable the listener to ask a question that prompts the family to elaborate more on the problem
- Gives the family the opportunity to discuss key aspects of the problem in depth
- Gives the listener the opportunity to elicit specific examples and expand on details and relevant information.
Make sure to listen carefully. Sometimes we are guilty of automatically formulating the next question or resorting to a predetermined answer without paying attention to what the speaker is actually saying.
| Open-Ended Questions | Closed-Ended Questions |
|---|---|
| Tell me about your relationship with your sister? | Do you get along with your sister? |
| What types of things did you and Joe talk about when dealing with these types of situations? | Have you ever talked with Joe about these types of circumstances? |
| When did you last spend time with your cousin? | Do you have any happy memories of your cousin? |
| What interests do you and your brother share or do not share? | Do you have the same interests as your brother? |
| How may/can I help you? | Can I help you? |
| Other open-ended examples: Can you give me an example? What are your feelings about that? How was that for you? |
| Family | Response Using Open-Ended and Reflective Listening |
|---|---|
| I just don’t know what to do… | It sounds like you are struggling with what steps to take next… Pause. If no response, what have you done in the past when you don’t know what to do? |
| We never talked about it, so I cannot make a decision for him. | As his wife of 15 years, the one who brought him lunch every Friday, and accompanied him to all those rainy-day soccer games… what do you think your conversation would have looked like had you been able to talk about it? or How did he make decisions for himself? |
| I want this to be over asap! It’s just too painful. | I can hear that this is very hard for you. What do you imagine the next 24 hours looking like… so that I can help? |
| Everything is happening too fast and I need more time to figure things out. | So many things are happening for you and your family. Tell me about what is most important for you right now. |
| If family is silent but visibly upset with the conversation. | Ms. Smith, you appear upset by what I just said… pause and wait for a response. Or I get the impression that something I said caused a reaction in you… pause and wait for a response. |
| They say he’s brain dead, but I don’t believe it. | I can see that you still have questions about the brain death declarations that were completed this morning; could you tell me more about that? |
If a family is not able to immediately share, try narrowing your questions and then make them broader as the conversation goes on. For example, if you ask “What questions do you have about what the doctor said regarding brain death?”; if the family has none, you can narrow your questions by asking, “For some families, being told their loved one is brain dead while they remain on ventilated support, feel warm, and look like they’re sleeping is difficult and sometimes confusing… what were your initial thoughts about this?”
These guidelines are not meant to be a script, but a guide with examples on how to utilize reflective listening and open-ended questions to engage a grieving family in a quality, genuine, and compassionate conversation so that they are able to make the best decisions for their loved one.
Example 3: Donation Conversation Scripts
My husband never wanted to be on life support. I want him to be removed from the ventilator.
I hear that you are saying your husband never wanted to be on life support, it must be difficult for you to see your husband this way. I respect that you want to remove the ventilator and support your husband’s wishes. But before that happens, I’d like to talk to you about an opportunity that your husband has because he is on the ventilator. I understand his point of view as I myself would not wish to remain on a ventilator. Did your husband have any opinions regarding donation? Your husband can help others. Your husband would only have tolerated ventilator support long enough to start the donation process.
My daughter has been through enough. I don’t want her cut on.
Your daughter has been through so much, and your concerns about her body are very appropriate. You are looking out for her best interest and we want to do the same for her and for her family. Unfortunately, no one can change all that she’s had to go through, but donation could change this terribly devastating situation into an opportunity of life for other families who are on the verge of having to deal with the same loss you have been faced with.
I’m sorry, but I just want my wife to be whole when we bury her.
I am sorry you are going through this tough time. Many families have found comfort in knowing their loved one’s organs were transplanted to save the lives of others. Many lifesaving organs are destroyed during preparation for funeral viewings and autopsies by medical examiners. Many families are unaware the vital organs are removed during these processes. Since the organs will be removed during these processes, we would like to offer you the chance to give someone life.
When my wife signed up on the donor registry, she did not know what she was signing up for. I know she would not want to go through all of this.
I must believe because your wife signed up that her intent was to give and help others, and that she would be willing to go through the process that takes to help save lives. I respect and fears and concerns you have and would like to address them so that you have peace with your wife’s decision.
It just takes too much time and we want to be done.
That is not an unusual response that we hear from families. You have going through a very traumatic event. You are tired and in shock. My job is to help support you through this time. One way of doing that is if you can to go home for a bit, to get a shower, lay down and rest, take care of things there and just not be here. We have families that take this time to plan the funeral or memorial service. You can know that your loved one is going to be cared for and we can keep you updated if you leave. Some families split the time up into shifts so people can have their own time with their loved one.
I heard about (___________) who was diagnosed brain dead and they’re fine.
You know, I’ve heard that before and what I’ve come to know is that sometimes, in trying to describe a bad head injury someone will use the term “brain dead”. It’s a misuse. Brain death is a specific diagnosis that means all, not just some, of the person’s brain cells have died. It is descriptive of why they died—their brain failed. Just like cardiac death means someone died because their heart failed.”