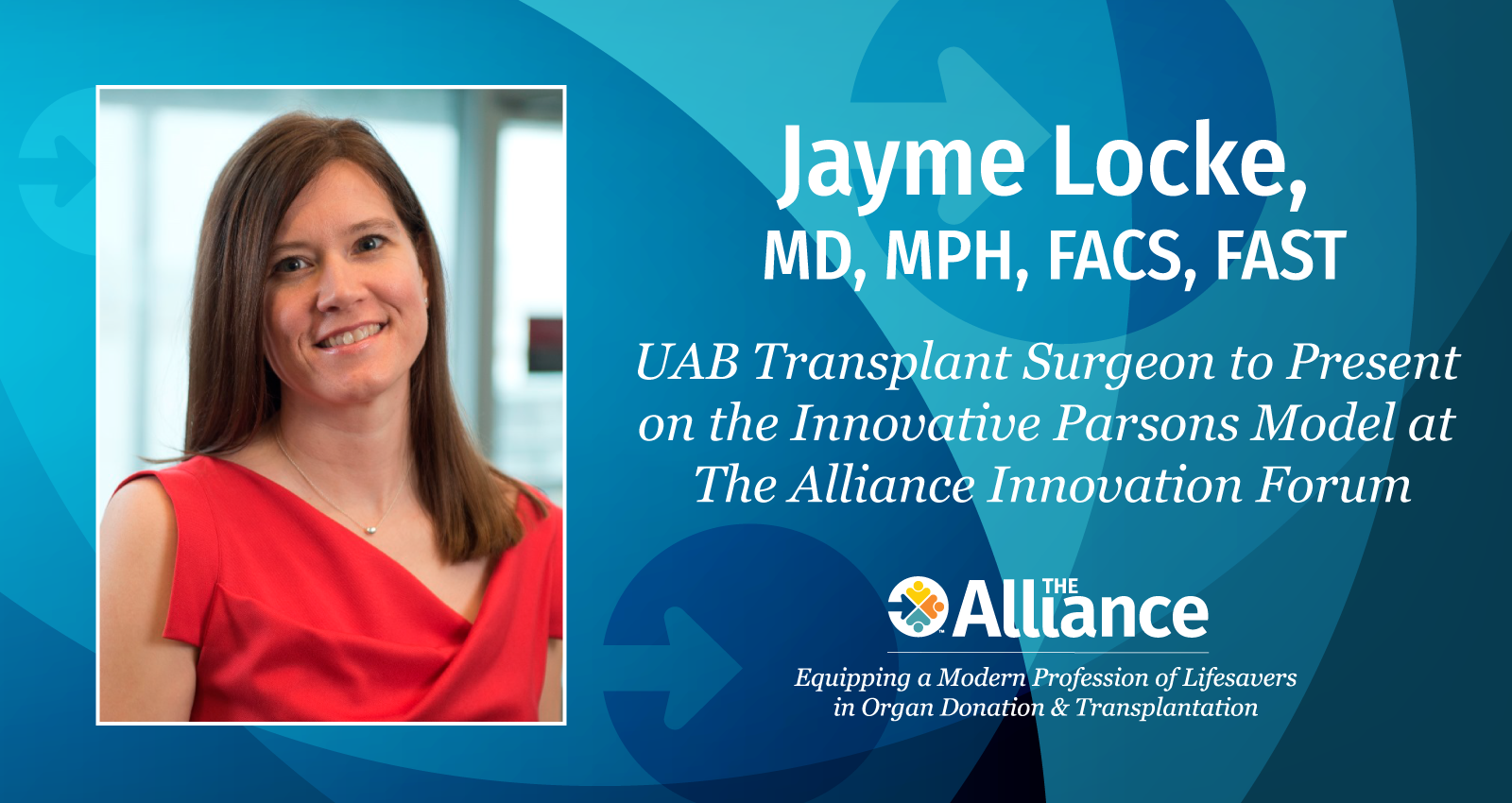
Innovation is important for solving challenging problems, says Dr. Jayme Locke, MD, MPH, FACS, FAST, an abdominal transplant surgeon who specializes in innovative strategies for the transplantation of organs. “My interest and involvement in xenotransplantation is centered around my interest in health equity,” says Dr. Locke. “It drives and motivates me and is something we need to try to achieve. In the setting of transplantation, xenotransplantation is an opportunity to introduce health equity by eliminating that gap between supply and demand.”
Dr. Locke, professor of Surgery and the Arnold G. Diethelm MD Endowed Chair in Transplantation Surgery at the University of Alabama Birmingham (UAB), took xenotransplantation a major step forward in potentially utilizing an alternative supply of organs for people facing life-threatening disease when she led a team on September 30, 2021, that successfully transplanted two genetically engineered pig kidneys into a deceased donor. Dr. Robert Montgomery, director of the NYU Langone Transplant Institute, had attached a kidney that remained outside the body from a genetically modified pig to a brain-dead individual a few days earlier. The UAB surgery was reported in The American Journal of Transplantation in January 2022, the first time a pig-to-human organ transplantation was described in a peer-reviewed medical journal.
Drs. Locke and Montgomery are among a group of innovators who will discuss their work at the Organ Donation and Transplantation Alliance’s (The Alliance) April 30 National Innovation Forum: The Future of Organs for Transplant, a one-day virtual forum that will explore alternative therapies to traditional human donor organ transplants.
Dr. Locke will provide an update on xenotransplantation during the session, and talk about the Parsons Model, named after James Parsons, the deceased man who received the modified pig kidneys at UAB in 2021. The Parsons model involves conducting xenotransplant surgery in brain-dead individuals who wanted to be organ donors for the purposes of research or transplantation, but for whatever reason, their organs could not be placed for transplant.
During the April forum, she will also show a video interview with Julie O’Hara, Mr. Parsons’ wife. “This has been an incredibly powerful journey for his family–a journey of healing, of hope, and of legacy for their loved one,” says Dr. Locke. “It has catapulted xenotransplantation into the realm of reality, which you’re now seeing unfold before our eyes with the world’s first successful transplant of a genetically-edited pig kidney into a man living with end-stage kidney disease at Massachusetts General Hospital in March 2024.”
Two-Year Journey to Develop the Parsons Model
Dr. Locke said that about 30 years ago, Dr. Tom Starzl, who is known as the father of liver transplantation, floated the concept of leveraging human brain-death individuals as a novel preclinical model.
“We wanted to make sure we did it correctly, because we did not want to interfere with the allotransplantation and with the typical donation process to somehow end up decreasing the number of organs available for transplant. We wanted to make sure that we weren’t prioritizing the science and our need for knowledge over the bereavement of families. We brought ethicists and all the key stakeholders to the table to make sure that we did this in a responsible and thoughtful way.” She says the Parsons model is an innovation that provides the opportunity to contribute to medicine and health care beyond xenotransplantation to test other new therapeutics.
“Sometimes it’s hard to go to sleep,” admits Dr. Locke. “I’m constantly trying to think of the next thing that will move the needle on getting everyone transplanted who needs an organ. We’ve showed that xenotransplantation can work in a preclinical human model but how do we move this into living people? We need an IND (investigational new device) to keep moving things forward to make a difference in patients’ lives.”
Passionate about Health Disparities Led to Xenotransplantation
 Dr. Locke grew up in eastern North Carolina; she lived with her mother in Goldsboro, where she attended school and spent the summers with her father on his farm in Aurora. She became interested in science while working at her father’s fish hatchery and she also wanted to help people, so she decided to become a doctor when she was 12 years old.
Dr. Locke grew up in eastern North Carolina; she lived with her mother in Goldsboro, where she attended school and spent the summers with her father on his farm in Aurora. She became interested in science while working at her father’s fish hatchery and she also wanted to help people, so she decided to become a doctor when she was 12 years old.
She attended Duke University and then East Carolina University medical school which is renowned for its primary care training. As a medical student, she worked in a blood pressure and diabetes screening clinic in the small community of Tillery, NC located in Hallifax County, which did not have a single physician and where 26 percent of the county’s population live in poverty, nearly twice the national average.
During that experience and as a medical student on surgical rotation, she was struck by the effects of the lack of care that she saw in many patients. “I remember thinking, ‘My God, we should try to do something about this and make the world better.’ I wanted to do research and try to move the needle not just for an individual patient, but for populations and that’s what took me to my MPH.”
“My health equity interest and my love of transplant stem from that time I spent in Tillery, NC seeing patients who already had end organ effects from their untreated diabetes and hypertension and seeing transplant as a cure, only to learn that we don’t have enough organs to go around. I saw xenotransplantation as a unique opportunity to make a difference.”
After the second year of her general surgery residency at Johns Hopkins, she decided to specialize in transplant surgery; she paused that training to do three years of research and earned a master’s degree in public health from Johns Hopkins, then completed her residency and did a postdoc fellowship in transplant surgery.
Translating from bench to the bedside
After completing her training, Dr. Locke was recruited to the University of Alabama Birmingham in 2012 to do health services research around health disparities. She also built and developed UAB’s incompatible kidney transplant program. She became involved in xenotransplantation in 2020 when Dr. Selwyn W. Vickers, dean of UAB’s Marnix E. Heersink School of Medicine, and Dr. Martine Rothblatt, founder and CEO of United Therapeutics, asked her to help translate it from the bench to the bedside.
Leading Collective Genius
Dr. Locke leads three teams at UAB:
- Transplant Epidemiology and Analytics in Medicine (TEAM) lab; the 25-member health services research team conducts complex statistical analyses that model transplant outcomes and practices and behavioral research that focuses on eliminating health disparities in transplantation;
- The 12-member Xenotransplant team; and
- A Clinical Care team of eight surgical partners who take care of patients.
She references the book, Collective Genius: The Art and Practice of Leading Innovation, when she talks about her approach to team leadership. “The lived experiences that people bring to the table provide unique perspectives that are important, particularly when you’re thinking about innovation,” she says. “You have to create a culture and an environment in which you can bring together talented people with different views and different lived experiences where they can each add their piece to the collective genius if you want to move the needle.”
“I have wonderful colleagues,” she continues. “It brings me so much joy to work with others to build these incredible programs and to see our patients benefit. It is extraordinary to give someone a transplant. It is extremely powerful when you see them after the transplant, and you look them in the eye, and you see for the first time hope restored because they have hope for a future that they did not think they were ever going to have.”
Father Taught her About Leadership
Locke played four varsity sports in high school; basketball, softball, track and field, and volleyball and says she learned some leadership skills as team captain, but that her father was her best teacher.
“My dad’s probably the greatest leader I’ve ever known,” says Dr. Locke. “He’s a retired airborne ranger colonel and from him I learned how to lead teams, how to deal with adversity, and how you lead through adversity. My dad is my best friend and he’s a great role model, mentor, and leader.” She frequently visits her father in North Carolina, and he visits her in Birmingham.

Dr. Locke has received numerous professional awards during her career and says she is proudest of the Dean’s Excellence Award in Mentoring she received in 2023. “Being a good role model and mentor and helping the next generation is critical,” says Dr. Locke. “It’s hard to become what you can’t see. It’s been very rewarding to mentor the next generation, particularly young women.”
She loves to travel and to hike and saw the Northern Lights in Iceland last year. She enjoys the symphony and opera; says she is obsessed with anything historical related to royalty on streaming services, and likes to read, enjoying books by Nicolas Sparks whose novels are set in her native eastern North Carolina
Hope Restored
“All of us who do transplant feel extremely privileged, because it really is miraculous,” says Dr. Locke. “That’s what motivates us all to figure out how to have the opportunity to offer a transplant to everyone who needs one. Everyone deserves that opportunity to have hope restored. We’ve got the secret sauce. We just don’t have enough to go around. We need more.”
“The hope is that someone can get an IND from the FDA; that’s really where we need to go if we want xenotransplantation to help us solve the organ shortage. It is theoretically possible to move all the way through the phases of an IND and have full approval in five years. It’s a tight timeline, but it is possible.”