The United States currently employs an opt-in donation system, but many have questioned whether the U.S. should move to an opt-out donation system like many countries have. This decision, however, is not a simple one as the two systems may not be comparable from both legislative and cultural perspectives.
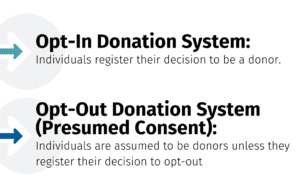 Under the Uniform Anatomical Gift Act (UAGA), the U.S. opt-in system allows individuals to register their legally binding decision to be a donor, that cannot be overturned by family or agents. The UAGA is based on the principles of Gift Law (e.g. wills and estate gifts) that can only be changed by the donor themselves, unless they are a minor.
Under the Uniform Anatomical Gift Act (UAGA), the U.S. opt-in system allows individuals to register their legally binding decision to be a donor, that cannot be overturned by family or agents. The UAGA is based on the principles of Gift Law (e.g. wills and estate gifts) that can only be changed by the donor themselves, unless they are a minor.
If an individual is not a registered donor, the decision to donate falls to the authorized legal party, most often Next of Kin (NOK) or legal agent, who make the decision whether to donate. Thus, the U.S. system provide two opportunities to request and act on the donation decision, first from the individual and second from the NOK/Agent, if no decision was recorded by the individual. In the U.S., a decision not to donate, is generally not recorded in state donor registries, but are routinely a legally binding option in each state’s Durable Power of Attorney for Healthcare (DPAHC). If there is a conflict between a DPAHC and a state donor registry decision, the most recent recorded decision prevails.
Most countries that have adopted an opt-out donation system, such as practiced in Spain, the U.K., Austria, and France, are founded on the legal notion that deceased donor organs are a public good and as such, may be legally recovered for transplant without specific authorization of the individual or family, unless the individual has recorded a decision not to donate upon death. In reality, countries with “opt-out” systems routinely do not operate donor registries nor non-donor registries, however these countries routinely seek family authorization at the time of death. Such systems are considered to be “soft” opt-outs.
One of the newest opt-out countries, the U.K., has sought to keep its donor registry by encouraging individuals to opt-in or to opt-out of donation by registering their decision. However, either decision can be changed if the family or legal proxy has newer information that indicates a change in the individual’s thoughts surrounding their decision to donate. Within the opt-out systems, a donation conversation will be initiated with the family to determine the patient’s wishes, regardless of their registered decision. If the patient has not registered their wishes, the donation conversation is approached with the assumption that he or she is a donor, however, the family can object to donation.
Which system is better? This question does not have a black and white answer.
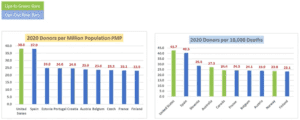
(Data Credit – IRODAT Organ Donation Data, shared by Tom Mone, OneLegacy)
The data demonstrates that the U.S. system is currently leading in donors per million and donors per deaths. Nonetheless, it is apparent that there is not a ‘one-size’ fits all system. Each country must examine which system best aligns with their political-structure, culture, and legislative oversight.
Culturally, the U.S. tends to value individual rights in its laws and social practices more than many countries and to exhibit a more skeptical attitude towards the government, so it seems appropriate to promote a system that focuses on personal autonomy and encourages individuals to legally register their wishes and to have those decisions protected through legislation.
Ultimately, neither system is a “one-size-fits-all” answer to ending deaths on national waitlists. The unfortunate reality is that even with more registered donors, the waitlists could be longer given that fewer than 1% of all deaths enable medically viable organ donors. Therefore, while it is imperative that deceased donation is optimized, patients on the waitlist will also need the help of the millions of others here in the US and around the world who could be considered for living donation.